Purpose
The Integrated Behavioral Health reviews and streamlines existing research and resources related to integrated behavioral healthcare (IBH). This webpage is for current and prospective students, providers, consumers, educators, policy-makers, and anyone interested in IBH.
Here you will find information on programs, practices, conferences, and scholarships related to integrated behavioral health - all in one place! You will also find educational and training materials, such as webinars, videos, and certificate programs. The University of Montana offers several courses that relate to IBH and you can find information on how these courses fulfill the competency requirements in the field. You will also find broader state and national IBH initiatives.
This webpage functions to make existing IBH-related resources more accessible and easier to interact with so that you can consult, borrow, and share information as you see fit.
To begin, take a look at Featured Resources for quick access to already-existing resource libraries and webinar trainings. If you want access to resources for a specific condition or population, click on Resources by Topic
Thank you for your interest in IBH initiatives at the University of Montana and across the state and nation!
About Behavioral Health
"A practice team of primary care and behavioral health clinicians, working together with patients and families, using a systematic and cost-effective approach to provide patient-centered care for a defined population. This care may address mental health and substance abuse conditions, health behaviors, including their contribution to chronic medical illness, life stressors and crises, stress-related physical symptoms, and ineffective patterns of health care utilization” (Peek, 2013).
The term behavioral health refers to an interdisciplinary, holistic focus on the relationships between the “mind” and the “body.” Instead of seeing physical and mental illnesses as separate entities that need to be treated singularly in separate settings, behavioral health focuses on the mind-body connection, and how, often, physical and mental health issues may be connected. Behaviors like our eating habits, legal and illegal drug use, and exercise routines can impact our physical health immediately or over a long amount of time. Some of these behaviors are under a person’s control, like their stress level or how much they eat or drink. However, some of these behaviors are not under our control, such as the pollution level of the environment that we live in or genetic factors that may contribute to obesity, anxiety, or depression.
Many conditions develop from both biological factors and our own personal environments or experiences. Indeed, mental and physical health issues often co-occur or are comorbid with each other. For example, often people who are diagnosed with diabetes often develop depression as well. Behavioral health aims to integrate primary physical health care with psychological services such as cognitive behavioral therapy or family therapy to help change the experience or the environment that the issues may occur in.
It is the goal of many psychologists and primary care professionals to integrate mental and physical health care into one setting. The ability to receive both mental and physical health treatment in one setting is helpful to reduce the stigma of receiving mental health services and to provide an ease of access to services for community members. It can be especially helpful since how we live our lives (behave) and our physical and mental health all interact with each other in complex ways.
Approximately 60% of patients with mental health issues seek care from primary care physicians rather than mental health professionals. Close to 2/3 of primary care physicians report difficulty finding mental health services for patients who need them. Lack of access to behavioral healthcare can result in overutilization of primary care services, poorer overall health outcomes, and higher provider burn-out and turnover rates.
These issues are significantly worse in rural areas with fewer providers, and for underserved patients with limited means. Rural Americans have higher rates of mental health and medical problems, more untreated mental health issues, greater barriers to care, and higher rates of suicide. Yet, residents of rural communities are less likely to receive vital mental and behavioral health treatment. In rural settings, like Montana, often one mental health center serves the entire county. It is difficult for community members to access necessary services and these difficulties are compounded by problems recruiting and retaining mental health providers. As a consequence, many rural Montanans seek behavioral care from their primary care providers.
Integrated behavioral healthcare (IBH) - where mental and physical health professionals work closely together to provide care for the whole patient – can address these problems. Healthcare models integrating physical and behavioral healthcare improve patient access to quality care. Furthermore, addressing mental and physical health needs simultaneously has demonstrated many advantages in some studies, including reducing hospitalization, increasing patient engagement, improving chronic disease care, raising outcomes, reducing errors, increasing provider job satisfaction, and lowering costs.
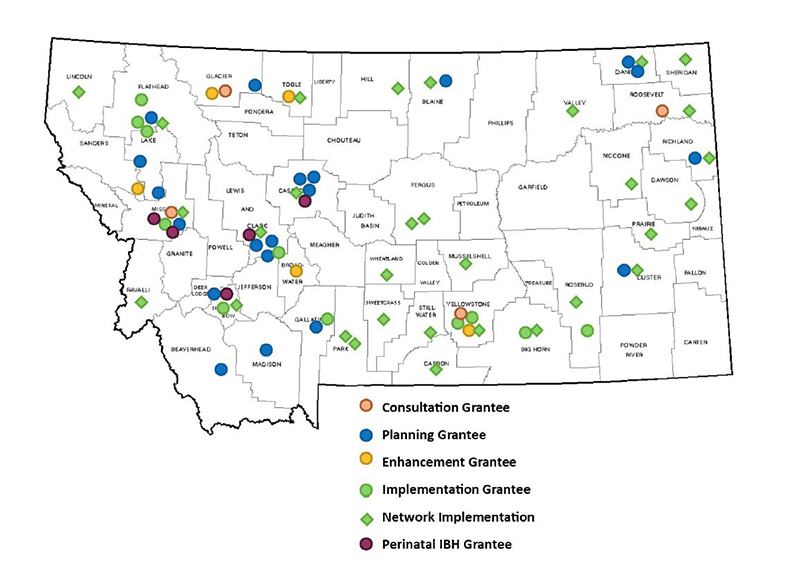
Integrated behavioral health is rapidly growing in the state of Montana. In the map below, you can see locations that are in the consultation, planning, enhancement, or implementation phases of integrated behavioral health services. IBH planning and implementation grants are available through the Montana Healthcare Foundation.
Learn more about IBH sites.
While the implementation of IBH has been shown to improve health outcomes and reduce health care costs, it has not been broadly implemented in many states – including Montana. Information from the Area Health Education Centers (AHEC) and the Montana Rural Behavioral Health Primary Care Collaborative (MRBHPCC) has shown that communities across Montana are looking for assistance in addressing mental health and behavioral health concerns in medical settings. Unfortunately, the practices and training requirements necessary to institute interdisciplinary partnerships have yet to be defined and developed fully. It is difficult to implement integrated behavioral healthcare models successfully, particularly in rural areas in Montana with scarce providers. Many integrated models presuppose the existence of supporting infrastructure and capacity, which are less likely to be present in rural settings.
Many of the online training resources available do not address the added challenges facing rural areas (e.g., distances, lack of public transportation, social isolation, confidentiality fears, caregiver stress and isolation). Further, few graduate programs have established comprehensive rural mental health training for their students. Behavioral health integration is vital for the success of healthcare reform and is currently lagging in its implementation.
In recent years, the University of Montana and the Area Health Education Centers (AHEC) have addressed this problem by placing psychology and social work trainees in rural communities to work on primary care teams. However, more work remains to be done to move toward an integrated healthcare model.
Hopefully information on this webpage will help communities in the state to build consultative relationships, as well as develop a curriculum for communities with similar needs.
The Annapolis Coalition on the Behavioral Health Workforce, under the auspices of the Center for Integrated Health Solutions (CIHS), created the Core Competencies for Integrated Behavioral Health and Primary Care. Divided into nine categories, these competencies provide organizations and individual professionals a “gold standard” for the skill set needed to deliver integrated care. They represent the long-term goal of workforce development for professionals with careers in integrated care. The core competencies provide a reference for the vision of an integrated workforce. Underneath each competency you will find current UM courses that provide training in that competency.
Core Competencies for Integrated Behavioral Health and Primary Care
Core Competencies for IBH and Primary Care
The ability to establish rapport quickly and to communicate effectively with consumers of healthcare, their family members and other providers.
Examples include: active listening; conveying information in a jargon-free, non-judgmental manner; using terminology common to the setting in which care is delivered; and adapting to the preferred mode of communication of the consumers and families served.
UM course offerings:
- PSYX 530 Clinical Interviewing
- PSYX 631 Motivational Interviewing
The ability to function effectively as a member of an interprofessional team that includes behavioral health and primary care providers, consumers and family members.
Examples include: understanding and valuing the roles and responsibilities of other team members, expressing professional opinions and resolving differences of opinion quickly, providing and seeking consultation, and fostering shared decision-making.
UM course offerings:
- PSYX 534 Applied Clinical Methods
The ability to conduct brief, evidence-based and developmentally appropriate screening and to conduct or arrange for more detailed assessments when indicated.
Examples include screening and assessment for: risky, harmful or dependent use of substances; cognitive impairment; mental health problems; behaviors that compromise health; harm to self or others; and abuse, neglect, and domestic violence.
UM course offerings:
- PSYX 525 Psychological Evaluation I
- PSYX 526 Psychological Evaluation II
- PSYX 532 Advanced Psychopathology
- PSYX 631 Neuropsychological Assessment
- PSYX 631 Substance Misuse
- PSYX 632 Introduction to Clinical Neuropsychology
The ability to create and implement integrated care plans, ensuring access to an array of linked services, and the exchange of information among consumers, family members, and providers.
Examples include: assisting in the development of care plans, whole health, and wellness recovery plans; matching the type and intensity of services to consumers’ needs; providing patient navigation services; and implementing disease management programs.
The ability to provide a range of brief, focused prevention, treatment and recovery services, as well as longer-term treatment and support for consumers with persistent illnesses.
Examples include: motivational interventions, health promotion and wellness services, health education, crisis intervention, brief treatments for mental health and substance use problems, and medication assisted treatments.
UM course offerings:
- PSYX 531 Principles of Psychological Intervention
- PSYX 535 Principles of Child Intervention
- PSYX 604 Psychological Intervention in Rural Integrated Behavioral Health
- PSYX 631 Behavioral Medicine/Clinical Health Psychology
- PSYX 631 Dialectical Behavior Therapy
- PSYX 631 Motivational Interviewing
The ability to provide services that are relevant to the culture of the consumer and their family.
Examples include: identifying and addressing disparities in healthcare access and quality, adapting services to language preferences and cultural norms, and promoting diversity among the providers working in interprofessional teams.
UM course offerings:
- PSYX 406 Rural Integrated Behavioral Health Care for Montana
- PSYX 631 Family Psychology
- PSYX 631 LGBT Issues
- PSYX 632 Advanced Multicultural Psychology
The ability to function effectively within the organizational and financial structures of the local system of healthcare.
Examples include: understanding and educating consumers about healthcare benefits, navigating utilization management processes, and adjusting the delivery of care to emerging healthcare reforms.
The ability to assess and continually improve the services delivered as an individual provider and as an interprofessional team.
Examples include: identifying and implementing evidence-based practices, assessing treatment fidelity, measuring consumer satisfaction and healthcare outcomes, recognizing and rapidly addressing errors in care, and collaborating with other team members on service improvement.
UM course offerings:
- PSYX 534 Applied Clinical Methods
The ability to use information technology to support and improve integrated healthcare.
Examples include: using electronic health records efficiently and effectively; employing computer and web-based screening, assessment, and intervention tools; utilizing telehealth applications; and safeguarding privacy and confidentiality
The work upon which this web site is based was funded through a grant awarded by the Montana Healthcare Foundation.

Disclaimer: The statements and conclusions on this site are those of the Grantee and not necessarily those of the Montana Healthcare Foundation. The Montana Healthcare Foundation makes no warranties, express or implied, and assumes no liability for the information contained on this site.
